A geriatric patient is unsteady after ambulating from a chair, a common issue that can indicate underlying health concerns. This article delves into the assessment, risk factors, interventions, and prevention strategies for managing this condition, providing healthcare professionals with a comprehensive guide to ensuring patient safety and well-being.
Understanding the causes and appropriate interventions for unsteadiness in geriatric patients is crucial for effective patient care. This article aims to provide a clear and concise overview of the topic, empowering healthcare professionals with the knowledge and skills to effectively manage this condition.
Assessment: A Geriatric Patient Is Unsteady After Ambulating From A Chair
The initial assessment of a geriatric patient who is unsteady after ambulating from a chair should include the following steps:
- Assess the patient’s level of consciousness and orientation.
- Obtain a history of the patient’s symptoms, including the duration and severity of unsteadiness, any associated symptoms (such as dizziness, lightheadedness, or palpitations), and any recent changes in the patient’s health status.
- Perform a physical examination, including a thorough neurological examination, to assess for any underlying neurological deficits that may be contributing to the unsteadiness.
- Measure the patient’s orthostatic vital signs (blood pressure and heart rate) to assess for orthostatic hypotension.
- Assess the patient’s hydration status by checking the skin turgor and mucous membranes for signs of dehydration.
Risk Factors, A geriatric patient is unsteady after ambulating from a chair
The common risk factors associated with unsteadiness in geriatric patients include:
- Age: The risk of unsteadiness increases with age.
- Polypharmacy: Taking multiple medications can increase the risk of drug interactions and side effects, which can contribute to unsteadiness.
- Impaired mobility: Patients with impaired mobility are more likely to experience unsteadiness when ambulating.
- Cognitive impairment: Cognitive impairment can affect balance and gait, increasing the risk of unsteadiness.
Interventions
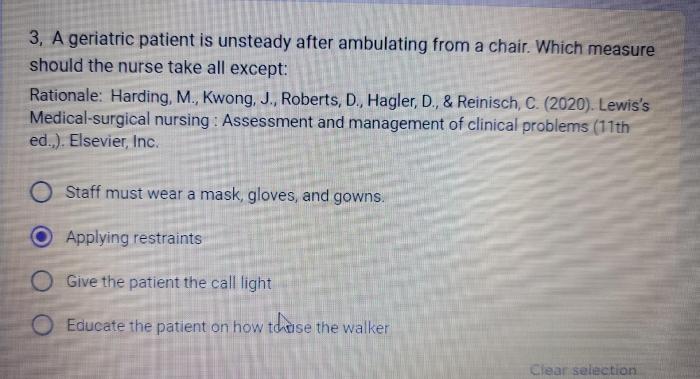
The immediate interventions for managing a geriatric patient who is unsteady after ambulating include:
- Safely assist the patient back to a seated position.
- Monitor the patient’s vital signs and level of consciousness.
- Provide reassurance and support to the patient.
- Optimize the patient’s hydration by providing fluids.
- Review the patient’s medications and make any necessary adjustments to minimize the risk of drug interactions and side effects.
Differential Diagnoses
The differential diagnosis for unsteadiness in geriatric patients includes:
| Diagnosis | Symptoms | Signs | Interventions |
|---|---|---|---|
| Orthostatic hypotension | Dizziness, lightheadedness, syncope | Decreased blood pressure and heart rate when standing | Increase fluid intake, elevate legs, consider medication adjustments |
| Dehydration | Thirst, dry skin and mucous membranes, decreased urine output | Elevated blood urea nitrogen and creatinine levels | Increase fluid intake, consider intravenous fluids |
| Neurological deficits | Weakness, numbness, tingling, loss of balance | Abnormal neurological examination findings | Referral to a neurologist for further evaluation and management |
Prevention
Fall prevention strategies for geriatric patients include:
- Exercise: Regular exercise can help to improve balance and strength, reducing the risk of falls.
- Balance training: Balance training exercises can help to improve the patient’s ability to maintain their balance.
- Environmental modifications: Making changes to the patient’s environment, such as installing grab bars and removing tripping hazards, can help to reduce the risk of falls.
- Home safety assessments: A home safety assessment can identify potential hazards in the patient’s home and recommend modifications to make the home safer.
- Assistive devices: Assistive devices, such as canes, walkers, and wheelchairs, can help to improve the patient’s mobility and reduce the risk of falls.
Essential FAQs
What are the common causes of unsteadiness in geriatric patients?
Common causes include orthostatic hypotension, dehydration, neurological deficits, cognitive impairment, and polypharmacy.
How can I safely assist a geriatric patient who is unsteady after ambulating?
Assist them back to a seated position, monitor vital signs and level of consciousness, and prevent further episodes by optimizing hydration and medication management.
What are the key strategies for preventing falls in geriatric patients?
Exercise, balance training, environmental modifications, home safety assessments, and assistive devices are essential for fall prevention.

